General medicine
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
A 24 year old male patient, from Srirampuram, presented to the opd with chief complaints of fever since 15 days which subsided on medication, cough & body pains.
History of present illness:
Patient was apparently asymptomatic 1 year back then he had yellowish discolouration of eyes for which he took herbal medication.
6 months back he again developed yellowish discolouration of eyes & was told red cells were less & administered Iron injections weekly once.
At present, patient had fever, cough.
H/o hemoptysis, Hematemesis.
H/o recent blood transfusion.
History of past illness:
The patient was not a known case of hypertension,diabetes mellitus,bronchial asthma,epilepsy & tuberculosis.No history of any surgeries.
Patient had delyed walking & delayed talking.
Personal history:
Mixed diet
Bowel & bladder - normal
Sleep- adequate
Family history:
No history of similar complaints in the family members.
General Examination:
The patient is conscious,coherant and cooperative.He is well oriented to time,place and person.
Pallor
No Icterus
No Cyanosis
No Clubbing
No Lymphadenopathy
Temperature - 36.1 °C
Pulse rate - 92/min
Respiration Rate - 16/min
Blood pressure- 100/60
SpO2 - 98%
Systemic examination:
CVS : S1 S2 +
Respiratory system: BAE +
Abdomen- scaphoid, no tenderness.
CNS- Conscious,Speech normal.
Provisional diagnosis- viral pyrexia with thrombocytopenia with anemia.
Investigations :
Haemogram:
Hb - 5.7 gm/dl
TLC - 4400 cells/cumm
PCV -17.4 vol%
RBC - 1.9 million/cumm
Platelet count - 1.20 lakh/cumm
Smear - Microcytic,Hypochromic Anemia with thrombocytopenia.
Complete Urine Examination:
Normal
Albumin - nil
Sugars -nil
Malarial parasite - negative.
ECG:
TPR Chart:
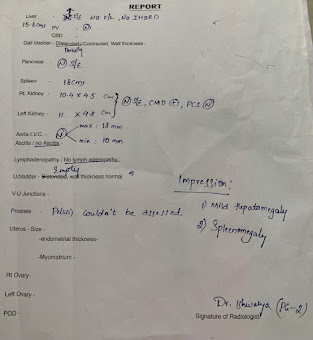
Ultrasound Report :
Liver Function Test:
Total Bilurubin - 2.09 mg/dl
Direct bilurubin -0.41 mg/dl
AST -30 IU/L
ALT -10 IU/L
Alkaline phosphate -112 IU/L
Total Proteins -6.1 gm/dl
Albumin -3.4 gm/dl
A/G ratio - 1.30
Renal Function Tests
Serum Creatinine-1.1 mg/dl
Blood urea - 27 mg/dl
LDH - 554
Serum electrolytes :
Sodium - 138 mEq/L
Potassium - 3.9 mEq/L
Chloride- 101 mEq/L
Questions :






Comments
Post a Comment